血清抗粒線體抗體陰性之原發性膽道性肝硬化:一病例報告
蔡元銘 周楠華1 鄭斌男 張定宗
國立成功大學附設醫院內科部 病理部1
摘要
原發性膽道性肝硬化以疲倦﹐發癢﹐肝腫大﹐黃疸及具有抗粒線體抗體等為特色。 我們發表一個具有抗粒線體抗體陰性的 55 歲女性病人,她具不正常的 肝功能,尤其是代表膽汁滯留的鹼性磷酸酵素和血清麩胺醯轉移。腹部超音波發現有肝硬化,但並無任何膽道擴張。 病理組織切片發現有膽管的漏失,門脈區 有淋巴球浸潤且有肉芽腫組織形成。 確切診斷是經過病理組織切片證實及升高的免疫球蛋白和抗核抗體。 因此,她開始接受膽鹽治療(12 毫克/公斤/天)。 十年之後,肝功能指數被控制住且回復到接近正常的濃度。(慈濟醫學2003; 15:347-351)
關鍵語:肝硬化,原發性膽道性肝硬化,抗粒線體抗體陰性原發性膽道性肝硬化
收文日期:92年2月14日,修改日期:92年3月19日,接受日期:92年6月9日
抽印本索取及聯絡地址:台南市勝利路138號 國立成功大學附設醫院內科部 張定宗醫師 --------------------------------------------------------------------------------------------------------------------------- 按此看南京军区临床肝病研究中心 原发性胆汁性肝硬化肝移植的时机和预後 ﹕http://mis.511511.com/news/2004/03-12/094158.htm
Primary Biliary Cirrhosis with Negative Anti-Mitochondrial Antibody: A Case Report
Yuan-Ming Tsai, Nan-Hwa Chou1, Pin-Nan Cheng, Ting-Tsung Chang
Department of Internal Medicine, Pathology1, National Cheng Kung University Hospital, Tainan, Taiwan ABSTRACT
Primary biliary cirrhosis (PBC) is characterized by fatigue, pruritus, or hepatomegaly, and by the presence of anti-mitochondrial antibody (AMA). We report on a 55-year-old female with PBC, but who was negative for AMA. She had elevated liver biochemistry, especially alkaline phosphatase (ALP) and gamma-glutamyl transferase (GGT), which in the indicate cholestasis. Abdominal sonography revealed liver cirrhosis with no evidence of biliary tract dilatation. Liver pathology showed loss of the bile duct, lymphocyte infiltration within portal areas, and granuloma formation. The diagnosis of PBC was confirmed by pathologic findings in addition to immunoglbulin (Ig) M and antinuclear antibody (ANA). She received oral ursodeoxycholic acid at a dosage of 12 mg/kg/day. After 10 years of treatment, liver function has been well controlled, and she has nearly normal liver biochemical tests. (Tzu Chi Med J 2003; 15:347-351)
Key words: cirrhosis, primary biliary cirrhosis, anti-mitochondrial antibody
Received: February 14, 2003, Revised: March 19, 2003, Accepted: June 9, 2003
Address reprint requests and correspondence to: Dr. Ting-Tsung Chang, Department of Internal Medicine, National Cheng Kung University Hospital, 138, Sheng Li Road, Tainan, Taiwan
INTRODUCTION
Primary biliary cirrhosis (PBC) has traditionally been regarded as a severe but uncommon disorder that progresses slowly and silently to cirrhosis [1,2]. It usually affects middle-aged women with the diverse pres-entations of fatigue and pruritus, hepatomegaly of unknown origin with cholestasis, or a high serum level of alkaline phosphatase (ALP). The diagnosis is confirmed by the presence of anti-mitochondrial antibody (AMA) and by the pathology. However, a minority of patients have all of the histological, biochemical, and clinical manifestations that are consistent with PBC but are persistently AMA-negative [1].
The natural history and associated autoimmune conditions in AMA-positive and AMA-negative PBC appear to be exactly the same. However, because the auto-antibody profile of AMA-negative PBC is similar to that of autoimmune hepatitis, a careful review of the liver biochemical pattern and histology is necessary [3].
Herein, we report on a case of AMA-negative PBC, in which the diagnosis was made and confirmed by clinical manifestations and pathologic findings under ursodeoxycholic acid (UDCA) treatment.
CASE REPORT
A 55-year-old female came to the Family Medicine Outpatient Clinic with symptoms of fatigue, general weakness, and pruritus for 2 weeks in 1989. The liver biochemical tests showed elevated aspartate aminotransferase (AST) at 41 U/L (normal, 5-40 U/L), alanine aminotransferase (ALT) of 235 U/L (normal 0-55 U/L), alkaline phosphatase (ALP) of 256 U/L (normal, 30-110 U/L), and gamma-glutamyl transferase (GGT) of 1678 U/L (normal, 8-80 U/L) (Table 1), but a normal bilirubin level. Her condition worsened in the subsequent 2 years of follow-up.
In 1991, she visited the Gastroenterology Outpatient Clinic. Further tests were negative for HBsAg, anti-HCV antibody, and AMA, and showed a reverse ratio of albumin (3.7 mg/dL) versus globulin (4.4 mg/dL), as well as immunoglobulin (Ig) G of 1990 mg/dL (normal, 810-1690 mg/dL), IgM of 408 mg/dL (normal, 60-280 mg/dL), and IgA of 472 mg/dL (normal, 90-450 mg/dL). Abdominal sonography revealed liver cirrhosis with no evidence of biliary tract dilatation (Fig. 1). A liver biopsy was then performed, and portal areas showed lymphocytic infiltration, piecemeal necrosis, loss of the bile duct, and granuloma formation (Fig. 2).
Under the impression of primary biliary cirrhosis, UDCA at a dosage of 12 mg/kg/day was prescribed for this patient. ALT and AST levels decreased from 124 and 122 U/L, respectively to normal limits. ALP and GGT values decreased from 569 and 2076 U/L, respectively to nearly normal levels within the following 10 years. Cholesterol levels of around 400 mg/dL decreased to within normal limits 2 years later and were maintained even without the use of cholesterol-lowering drugs (Table 1). She was positive for the antinuclear antibody (ANA) with a titer of > 1:2560 (+) in a centromere pattern and 1:40 (+) in a homogeneous pattern, but no other autoimmune diseases were found in the patient. There was also no recurrence of abnormal liver function in the regular follow-up.
DISSCUSSION
Primary biliary cirrhosis (PBC) is a chronic liver disease. Previous reports have suggested that 90% of patients are female and most of them are around 40 years of age [1,2]. The clinical presentations of PBC include persistent fatigue (80%), pruritus (50%-60%), hyper-pigmentation, xanthelasmata, and hypercholester-olemia. The classic triad of diagnosis of PBC is positive AMA, cholestasis-type liver biochemistry, and histological characteristics. In addition, extrahepatic biliary obstruction should be excluded. PBC is also associated with autoimmune disease. Despite the high prevalence of hypercholesterolaemia, patients with PBC are not exposed to a higher risk of cardiovascular events than the general population. It is estimated that 40%-100% of patients are symptomatic and will subsequently develop symptoms. The level of bilirubin only rises in a minority of patients or in the later stage of the disease [1,4-6].
The pathologic features of PBC can be separated into 4 stages. In the first stage, destructive cholangitis is predominant. In the second stage, bile duct damage with ductal loss and adaptive proliferation in residual ducts is present. Hepatocytes also reveal cholestatic features adjacent to the portal tracts. In the third stage, necrosis of hepatocytes and bridging fibrosis are the predominant changes. In the last stage, biliary cirrhosis is present and hepatocytes preserve their acinar structure. Patients in the first and second stages show better responses to UDCA [7].
Regarding the differential diagnosis of primary sclerosing cholangitis (PSC), PSC shows bile ducts loss, but rarely granulomas. Previous reports reveal that 50% of PBC patients had bile duct loss and 40% of patients had granulomas [7,8]. The presence of granulomas in PBC seems to be of better prognostic significance [8]. In this case, both bile duct loss and granulomas were present. Therefore, the impression was primary biliary cirrhosis, in stage II through pathologic examination.
Early studies of PBC demonstrated that up to one third of patients with PBC had serum antibodies directly against nuclear autoantigens (ANAs) [6,9]. A small minority of patients have all of the histologic, biochemical, and clinical feature of PBC but are persistently negative for AMA. Most patients with PBC are ANA-positive. The term "autoimmune cholangitis" has recently been coined to describe those AMA-negative patients who are positive for ANA and who possess granulomatous cholangitis. Autoimmune cholangitis appears to run a similar clinical course as "classical" PBC [2,6,10]. In a previous study, antinuclear and anti-smooth-muscle antibodies, as well as lower serum IgM and ALT, were more common in the AMA-negative group compared to the AMA-positive group. However, no difference was found between AMA-negative and AMA-positive patients with respect to age, gender, biochemical features, and medical response [11,12].
The treatment of PBC has 2 major aims: (a) to slow down the disease progression, and (b) to alleviate symptoms of PBC, such as pruritus and fatigue. Liver transplantation is the last choice [1,13].
Two types of drugs can be used to slow down disease progression: exogenous hydrophilic bile acids (i.e, UDCA) or immunosupressants. UDCA was reported to increase bile flow, reduce stagnation, and modify bili-ary epithelial HLA expression. It has a greater effect on pruritus (40%), but little effect on fatigue. Whether it can prolong survival or not is controversial [14,15]. Immunosupressants include penicillamine, azathioprine, MTX, cyclosporin, colchicine, and steroids [1,16].
In conclusion, UDCA is helpful for the treatment of mild PBC in the long-term course, but its benefit in terms of mortality needs further evaluation. AMA-negative PBC has similar clinical presentations, laboratory results, pathologic features, and treatment modality as AMA-positive PBC. It should be suspected in patients with pruritus and elevated values of ALP and GGT. A liver biopsy is recommended for confirmation of the diagnosis.
REFERENCES
1. Prince MI, Jones DE: Primary biliary cirrhosis: New perspectives in diagnosis and treatment. Postgrad Med J 2000; 76:199-206.
2. Kaplan MM: Primary biliary cirrhosis: Past, present, and future. Gastroenterology 2000; 123:1392-1394.
3. Zhang F, Jia J, Wang B, et al: Clinical characteristics of primary biliary cirrhosis: A report of 45 cases. Zhonghua Nei Ke Za Zhi 2002; 41:163-167.
4. Prince M, Chetwynd A, Newman W, Metcaff JV, James OF: Survival and symptom progression in a geographically based cohort of patients with primary biliary cirrhosis: Follow-up for up to 28 years. Gastroenterology 2002; 123:1044-1051.
5. Talwalkar JA, Keach JC, Angulo P, Linder KP: Overlap of autoimmune hepatitis and primary biliary cirrhosis: An evaluation of a modified scoring system. Am J Gastroenterol 2002; 97:1191-1197.
6. Longo M, Crosignani A, Battezzati PM, et al: Hyperlipi-daemic state and cardiovascular risk in primary biliary cirrhosis. Gut 2002; 51:265-269.
7. Degott C, Zafrani ES, Callard P, Balkau B, Poupon RE, Poupon R: Histopathologic study of primary biliary cirrhosis and the effect of ursodoxycholic acid treatment on histology progression. Hepatology 1999; 29:1007-1021.
8. Lee RG, Epstein O, Jauregui H, Sherlock S, Scheuer PJ: Granulomas in primary biliary cirrhosis: A prognostic feature. Gastroenterology 1981; 81:983-986.
9. Joshi S, Cauch-Dudek K, Wanless IR, et al: Primary biliary cirrhosis with additional features of autoimmune hepatitis: Response to therapy with ursodeoxycholic acid. Hepatology 2002; 35:409-413.
10. Kim WR, Ludwig J, Lindor KD: Variant forms of chole-static diseases involving small bile ducts in adults. Am J Gastroenterol 2000; 95:1130-1138.
11. Lacerda MA, Ludwig J, Dickson ER, Jorgensen RA, Lindor KD: Antimitochondrial antibody-negative primary biliary cirrhosis. Am J Gastroenterol 1995; 90:247-249.
12. Michieletti P, Wanless IR, Katz A, et al: Antimitochondrial antibody negative primary biliary cirrhosis: A distinct syndrome of autoimmune cholangitis. Gut 1994; 35:260-265.
13. Tinmuth J, Tomlinson G, Heathcote EJ, Lilly L: Benefit of transplantation in primary biliary cirrhosis between 1985-1997. Transplanatation 2002; 73:224-227.
14. Corpechot C, Carrat F, Bonnand AM, Poupon RE, Pou-pon R: The effect of ursodeoxycholic acid therapy on liver fibrosis progression in primary biliary cirrhosis. Hepatology 2000; 32:1196-1199.
15. Corpechot C, Carrat F, Poupon R, Poupon RE: Primary biliary cirrhosis: Incidence and predictive factors of cirrhosis development in ursodiol-treated patients. Gastroenterology 2002; 122:652-658.
16. Weyman RL, Voigt M: Consecutive occurrence of primary biliary cirrhosis and autoimmune hepatitis: A case report and review of the literature. Am J Gastroenterol 2001; 96:585-587.
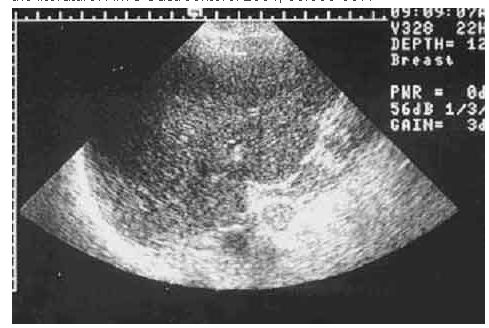
Fig. 1. Abdominal echo of the liver showing an uneven surface and normal caliber of the common bile duct.
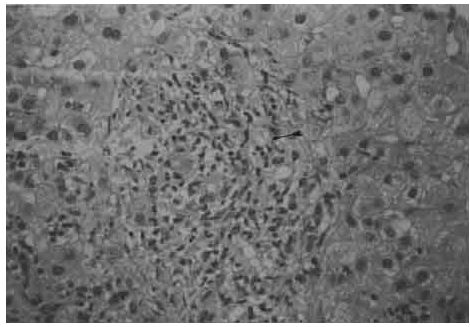
Fig. 2. Liver biopsy revealing piecemeal necrosis, focal necrosis, a portal area with bile duct loss, and granulomas (arrow).
Table 1. Biochemical Data of AMA-Negative Patients with PBC
Date | Albumin | Globulin | AST | ALT | Bil-T | Bil-D | ALP | GGT | Chol | | NL | 3-5(g/dL) | 5-40(U/L) | 5-55(U/L) | 0.2-1.4(U/L) | 0-0.4(U/L) | 30-110(U/L) | 8-80(U/L) | 131-300(mg/dL) | '89/5/27 | 4 | 4.5 | 141 | 235 | 1.1 | 0.6 | 256 | 1678 | | '90/11/7 | 4 | 4.6 | 130 | 142 | 0.9 | | 565 | | 372 | '91/1/10 | 3.7 | 4 | 209 | 192 | 0.5 | 0.1 | 525 | 1756 | 323 | '91/11/5 | 4.1 | 4.8 | 166 | 151 | 1 | | 601 | | 447 | '91/12/27 | 3.7 | 4.4 | 122 | 124 | 0.6 | | 565 | 2076 | | '92/4/2 | 4.3 | 4 | 98 | 99 | 0.9 | 0.3 | 492 | 1365 | 429 | '92/10/7 | 4 | 5 | 87 | 66 | 0.9 | 0.4 | 373 | 808 | 372 | '93/7/6 | 4.1 | 4.7 | 83 | 63 | 1.2 | 0.7 | 296 | 658 | 363 | '94/10/6 | 3.8 | 4.7 | 73 | 58 | 0.5 | 0.3 | 245 | 484 | 378 | '95/6/14 | 4 | 4.8 | 92 | 75 | 0.8 | 0.3 | 274 | 505 | 337 | '96/8/26 | 3.7 | 5.3 | 75 | 47 | 1 | 0.5 | 259 | 391 | 277 | '97/3/10 | 3.4 | 4.7 | 82 | 50 | 0.8 | 0.3 | 232 | 296 | 280 | '98/8/17 | 3.6 | 5.1 | 63 | 37 | 0.8 | | 247 | 194 | 196 | '99/4/19 | 3.5 | 5.3 | 69 | 42 | 0.7 | | 185 | 144 | 200 | '00/4/11 | 3.6 | 5.2 | 58 | 33 | 0.9 | | 155 | 133 | 182 | '01/11/19 | 3.5 | 5.3 | 58 | 37 | 0.8 | | 160 | 120 | 194 | '02/2/6 | 3.4 | 5.3 | 63 | 37 | 0.8 | | 160 | 105 | '02/5/20 | 3.5 | 5.5 | 51 | 29 | 0.8 | | 137 | 97 | '02/8/19 | 3.3 | 4.8 | 49 | 28 | 0.8 | | 129 | 86 |
NL: normal limits; AST: aspartate aminotransferase; ALT: alanine aminotransferase; Bil T: total bilirubin; ALP: alkaline phosphatase;
GGT: gamma-glutamyl transferase; Chol: cholesterol
http://www.tzuchi.com.tw/file/tcmj/92-5/9.htm |